Bearing the BAD NEWS
MARY OZENGHAR’S SURGEON didn’t waste any time delivering the news. Minutes after finishing Ozenghar’s breast biopsy, she told the 60-year-old human resources manager, “I don’t want you to leave here and think you’re OK,” Ozenghar recalls. “I know what cancer looks like and I think this biopsy’s going to come back positive.” Ozenghar was stunned, of course. But she appreciated the surgeon’s honesty.
“She told me ‘This is what we think you have and this is what we’re going to do’,” she says. “Not knowing is hard and not knowing what’s going to happen next is worse.”
But Ozenghar’s meeting with her oncologist was not nearly as reassuring. In fact, she says, “It was one of the worst doctor experiences I’ve ever had.”
The cancer doctor simply rattled off grim statistic after grim statistic during a curt meeting, Ozenghar says.
“I just sat out in the car and cried for half an hour,” she recalls. “It was so terrifying to have someone treat me like I was a piece of meat and a statistic.”
So, she found a new oncologist, one who spent two hours discussing her diagnosis and treatment options.
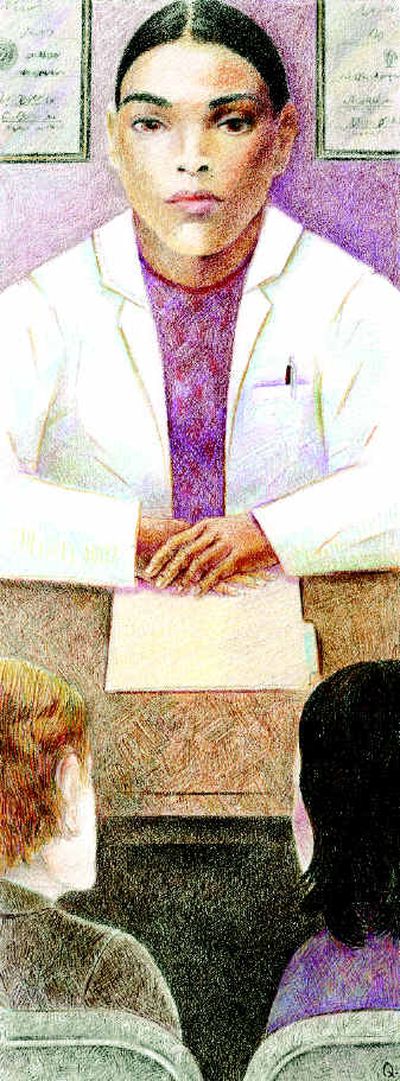
Doctors must break bad news to patients hundreds, if not thousands, of times during their careers. But many receive little or no training in how to deal with such uncomfortable situations. In fact, one survey found that fewer than 20 percent of oncologists had received any education in how to deliver distressing information.
“We really are part of a death-denying culture,” says Dr. J. Randall Curtis, director of Seattle’s Harborview End-of-Life Research Program. “Doctors, just like everybody else, have a hard time bringing up these topics … Academic medicine got its start trying to prove it could make people better. In fact, you can’t save everybody’s life.”
Barely a generation ago, doctors routinely withheld bad news from their sickest patients.
As a young doctor in the early 1970s, Dr. Robert Buckman watched a woman die of myeloma, a bone marrow cancer, while doctors told her little about her condition.
“In those days, nobody knew how to tell her,” Buckman says. “Everybody avoided telling her what was going on. As her suffering increased, we sort of didn’t go into her room very much. She was isolated.”
Buckman, now an oncologist at Princess Margaret Hospital in Toronto, watched how nurses communicated with dying patients and, over the years, he fashioned his own methods for breaking bad news.
In 1992, Buckman co-wrote “How to Break Bad News: A Guide for Health Care Professionals,” in which he details a protocol for talking with patients and their families.
“The basic message is before you tell, ask,” Buckman says, emphasizing that doctors should be as good at listening as they are at talking. “If you run away, they’ll never forgive you,” he says. “If you do it right, they’ll never forget you.”
By listening, doctors are able to find out what the patient wants and needs. Some people, for example, are keenly interested in finding out how many months or years they have to live. Others don’t want to know.
But, if a patient asks for numbers, Buckman says, “I feel you are duty-bound to give them a ballpark figure.”
Curtis recently published a study based on taped conversations of family conferences in the intensive-care unit. He found that during those meetings, doctors spent 70 percent of the time talking and 30 percent of the time listening. Family satisfaction was directly related to the amount of time doctors spent listening.
“The majority of doctors are in this business because they do care about patients and families,” Curtis says. “We haven’t done a good job of training people how to show that.”
It is becoming increasingly common for medical students and residents to be taught communication skills.
At Spokane’s Internal Medicine Residency program, residents learn about delivering bad news in ethics conferences throughout the year, says program director Dr. Judy Benson. They also observe attending physicians talking with patients and participate in role-playing exercises to simulate difficult conversations.
“It’s not ever an easy thing to learn how to do,” says Benson, who says such training was uncommon when she was in medical school in the ‘80s. “I certainly think by the end of their three years of time here they’ve done it and watched it enough.”
But can you really teach empathy?
“Yes,” Buckman says. “Because what you’re teaching is the empathic response, which is a technique for acknowledging the emotions. You do not have to feel the emotion yourself, nor should you.”
Melody Biehl was 41 when she went in for her first mammogram. She had no family history of breast cancer, so she was devastated when she got a call — while sitting at her dining-room table — telling her she had cancer.
“You’re in shock and then you cry and you’re going, ‘why me?’” says Biehl, an administrative assistant in Spokane.
She had a mastectomy with reconstruction and hasn’t had a recurrence since the cancer was first detected in 1997.
Biehl considers herself lucky that she had sympathetic doctors who took time to explain her diagnosis and treatment. But, she says, doctors need to do a better job telling patients about support groups and other helpful programs.
“Women are just not getting the support they need,” she says. “They need to talk to someone that’s been there, done that.”
Ozenghar, who lives in Liberty Lake, had a lumpectomy in April and started chemotherapy in May. She’s had three of her six treatments. She’ll undergo radiation after the chemo.
She’s thankful she sought out a second oncologist after having such a negative experience with the first.
“Whether someone treats you with caring and nurturing is so important,” she says. “How they deliver what they deliver is huge.”