‘Super bugs’ may be proliferating
TRENTON, N.J. – Flesh-eating bacteria cases, fatal pneumonia and life-threatening heart infections suddenly are popping up around the country, striking healthy people and stunning their doctors.
The cause? Staph, a bacteria better known for causing skin boils easily treated with standard antibiotic pills.
No more, say infectious disease experts, who increasingly are seeing these “super bugs” – strains of Staphylococcus aureus unfazed by the entire penicillin family and other first-line drugs.
Until a few years ago, these drug-resistant infections were unheard of except in hospital patients, prison inmates and the chronically ill. Now, resistant strains are infecting healthy children, athletes and others with no connection to a hospital.
“This is a new bug,” said Dr. John Bartlett, who chairs the committee on antibiotic resistance at the Infectious Diseases Society of America. “It’s a different strain than in the hospital … more dangerous than other staph.
“Primary care physicians and ER doctors, they don’t all know (about this) and should,” he said.
Bartlett, a professor at Johns Hopkins University School of Medicine, treated three young Baltimore area women this year who got pneumonia from this community-acquired resistant staph.
All had to be put on breathing machines, and one died, he said.
The infections will be a hot topic at the society’s annual meeting this week in Boston. The group has been warning that drug companies aren’t developing enough new antibiotics to avert a crisis.
Among the case reports to be discussed:
•In Los Angeles, doctors at UCLA Medical Center treated 14 people with necrotizing fasciitis, informally known as “flesh-eating bacteria,” over a 14-month stretch through April. Three needed reconstructive surgery and 10 spent time in intensive care.
“This is about as serious an infectious disease emergency as you can get,” said Dr. Loren G. Miller. “We don’t know how these people got the infection — there doesn’t seem to be a common thread.”
•In Corpus Christi, Texas, doctors at Driscoll Children’s Hospital saw fewer than 10 cases a year of community-acquired resistant staph infections in the 1990s, then saw 459 in 2003, with 90 percent in healthy children. Half were admitted to the hospital to get intravenous antibiotics; a few developed life-threatening lung and heart infections or toxic shock syndrome.
•A Centers for Disease Control and Prevention study shows another new twist: The resistant staph strain caused pneumonia in 17 people, killing five, during last year’s flu season. Only one had any risk factors for the infection.
“Nobody dreamt when we were in medical school that this would ever enter the community,” said Dr. Rajendra Kapila of University of Medicine and Dentistry of New Jersey in Newark.
He has treated several patients with the infections at University Hospital there, including an itinerant golf caddie who kept getting abscesses on his neck until he landed in the hospital two years ago. Kapila linked the infections to abrasions from the man’s golf bag strap.
In August, a man in his 40s with severe back pain turned out to have such a severe staph infection in his spinal cord and was paralyzed permanently, Kapila said.
Dr. John Segreti, an infectious disease specialist at Rush University Medical Center in Chicago, estimates about 1 in 10 patients, some with prior health problems, die from the infections.
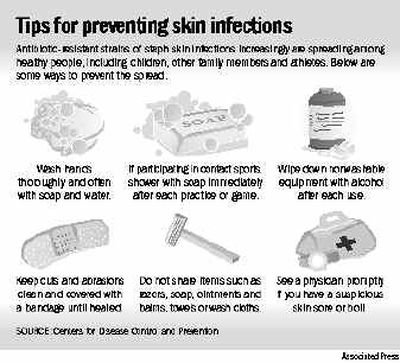
Dr. Dan Jernigan, a CDC epidemiologist, said athletes, children and military recruits are at higher risk. They are more likely to get cuts and scrapes and share close quarters and items such as towels and soap. Another factor is overuse of antibiotics, which tends to kill weak bacteria and help hardier ones develop resistance.
“Clinicians will have to think differently about skin infections,” Jernigan said. “We treat most skin infections without ever testing them.”
Testing will tell whether a strain is antibiotic-resistant, but the tests are expensive.
There are no national statistics on these infections, but health authorities are debating requiring doctors to report them.
CDC has reported on numerous infection clusters, including Colorado fencing club members, college football players in Pennsylvania and Los Angeles, and high school wrestlers in Indiana, and dozens of Pacific Islanders in Hawaii. Many patients were hospitalized, including most of the athletes. At least two outbreaks have occurred among Native Alaskans since 1996, with many cases linked to steam baths.
In New Jersey, infection clusters were reported in 2003 and earlier this year involving two high schools and members of one family.
In Stafford, Texas, Janet Johnson’s 13-year-old son Nicholas had such a severe infection — apparently after a minor football injury last October — that he was hospitalized for 5 1/2 weeks and nearly died. The staph infected his lungs, blood and bones, destroying hearing in one ear and making it difficult to walk.
“He was like a stroke victim,” she said, but he’s doing much better now thanks to extensive physical therapy, repeated surgeries and continuing use of antibiotics.