Who’s next? Long-term care facility residents, staff should get COVID-19 vaccinations this month

This week, some high-risk health care workers at Providence Sacred Heart Medical Center will get their second doses of the Pfizer vaccine, making them the first residents in Spokane County to be considered completely vaccinated against the novel coronavirus.
This landmark moment in the pandemic comes almost an entire year after the first case of COVID-19 in Washington, and in the United States, was confirmed in Snohomish County.
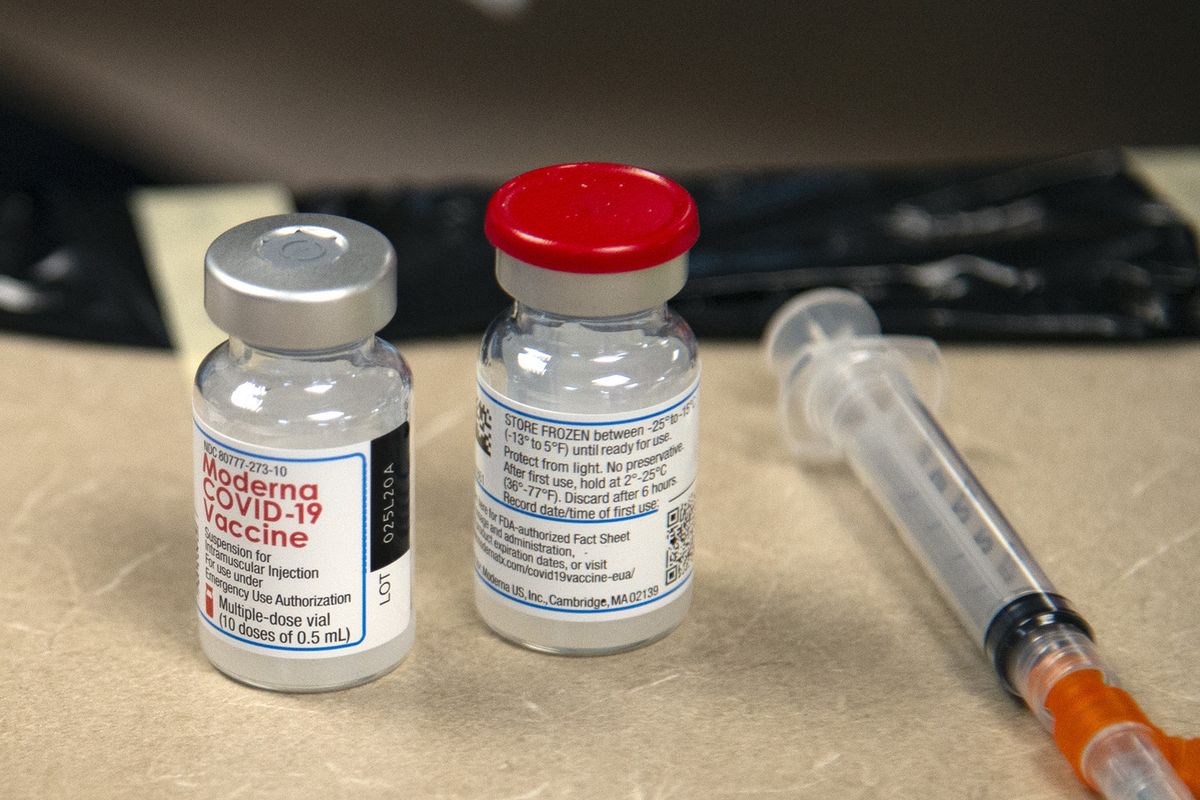
As the new year brings with it two vaccine candidates to fight the virus, high-risk health care workers and first responders are continuing to line up to get vaccinated this month. This group, along with long-term care facility residents and staff, should be offered the vaccine this month, according to the Washington Department of Health vaccination plan.
Thus far, the rollout of vaccination in Washington has been slower than anticipated due to myriad factors, state health officials acknowledged last week.
“Vaccination at this scale and on this timeline is a first and involves a lot of complex planning and logistics, and we’re continuing to look at how we can speed up the progress,” state Secretary of Health Dr. Umair Shah told reporters last Wednesday.
With the third wave of COVID-19 infections in Washington bringing with it record peaks in cases and hospitalizations, state health officials, following federal health guidance, prioritized frontline workers to get vaccinated first. This meant that many of the first facilities to receive and begin administering vaccine are the hospitals that are also taking care of the more than 1,000 hospitalized COVID-19 patients statewide.
As of last week, the federal government has allocated 522,550 doses of both the Pfizer and Moderna vaccine to Washington, and so far, 425,900 doses have been delivered.
Of those doses, hospitals and health care providers have administered 110,225 total doses since mid-December.
Of the state’s allocated doses, it must set aside about 96,000 for residents at long-term care facilities in the federal vaccination program for those facilities that opted in. The program connects CVS and Walgreens pharmacies to those facilities in order to vaccinate the residents and workers there. This program experienced delays at the federal level and did not formally begin until Dec. 28.
“There are 2,400 facilities, so all those phone calls to schedule and get visits can’t happen on the same day or week,” Michele Roberts, assistant secretary at the DOH leading the vaccine rollout, told reporters last week.
She said the department has worked with the pharmacies to prioritize skilled nursing facilities in their rollout to ensure the most vulnerable residents are vaccinated first.
While vaccine allocation to each state is determined by the federal government, the Department of Health decides exactly where those doses go in the state, telling the manufacturers where to ship them.
Currently doses are primarily going to hospitals and health clinics in order to vaccinate their frontline health care workers, who have been prioritized for the vaccine in Phase 1A of the state’s plan.
Not all health care workers eligible for the vaccination currently are working for organizations that are offering vaccines, and the state has advised employers to identify employees who are eligible to be vaccinated and write a voucher letter for them.
“We’re asking hospitals to help take on not just workers that are a part of their own system but also other health care workers,” Shah said last week. “So they are supportive of being able to do that, but there are logistical challenges they are working through.”
On Jan. 18, the state plans to roll out a “Phase Finder” tool, which will help individuals determine whether they are eligible for the vaccine. The tool will ask about a person’s age, work and level of risk when it comes to the virus. It will then determine in exactly what phase a person can be vaccinated. When you are eligible, it will tell you which providers locally in your county are offering vaccines, and how to contact them.
Late last week, the state released detailed guidance on who will be prioritized to receive the vaccine in the several tiers of Phase 1.
The first two tiers of Phase 1, called Phase 1A, include all workers in health care settings, first responders and long-term care facility residents and staff, an estimated 850,000 Washington residents. This group includes not only frontline nurses and doctors in hospitals but also behavioral health workers, school nurses and other workers who support health care operations on hospital campuses.
The state vaccination allocation plan estimates that these vaccinations will continue throughout January and maybe into February. Currently, there are still not enough vaccinations allocated to the state to complete vaccinating the number of residents in Phase 1A.
Both the Moderna and Pfizer vaccine require two doses, spaced four weeks and three weeks apart, respectively.
After frontline workers, prioritization for vaccines pivots to specific age groups. All Washington residents over the age of 70 and residents over the age of 50 who live in multigenerational households will be eligible to get a vaccine.
This group accounts for nearly 1.21 million Washington residents, according to department estimates, and it will likely take providers until the end of February or early March to complete vaccinating this group statewide.
State health officials used interviews and focus groups with hundreds of state residents and workgroups to decide who should get the vaccine first, prioritizing equity in how it is distributed.
The Department of Health is also prioritizing groups based on who the virus has most affected. People over the age of 60 account for 91% of the state’s COVID-19 deaths thus far in the pandemic.
Using scientific data of how the virus spreads and keeping equity in mind are both important, Maria Howard, an ethicist and assistant professor at Gonzaga University, said.
“We can’t let one get in the way of the other, even if we need them to work together,” she said.
She said the state’s prioritization appears to align with what we know about how the virus has disproportionately impacted communities of color thus far.
Nonwhite Washington residents have contracted COVID-19 and died at rates greater than white Washingtonians.
Native Hawaiians and Pacific Islanders have the highest case and hospitalization rates in the state, compared to white and Asian counterparts in Washington.
This was true even in a predominantly white community like Spokane County, where Marshallese residents this summer made up a third of confirmed cases in the region.
The reasons for this are many and varied, and Shah wrote in the vaccine allocation plan that there are economic, structural and social barriers that led to these inequities.
“The root causes of difference in COVID-19 cases, hospitalizations and deaths are due to longstanding systemic inequities, as are the differences in access to COVID-19 information, services and treatment in culturally and linguistically responsive ways,” the report says.
Howard said the data itself reveals the inequities.
“This is one of those situations where equity aligns with what the data are telling us in terms of how to move forward with vaccination, Howard said. “I think Washington’s equity focus has been genuine – it’s not perfect at all – but it’s been genuine.”
After older Washington residents are vaccinated, the allocation plan lists three more tiers of high-risk critical workers and residents who will be prioritized for vaccination. First, high-risk agriculture, grocery, food processing and child care workers, as well as K-12 educators and workers in other congregate facilities over the age of 50, will be offered the vaccine.
Then, people over the age of 16 with two or more comorbidities or underlying health conditions, including cancer, kidney disease and heart conditions, will get next priority.
Workers under the age of 50 in those same critical sectors and residents in congregate facilities, including prisons, group homes and shelters for people experiencing homelessness, will be eligible for the vaccine in the last tier of Phase 1.
These three last tiers of Phase 1B account for 1.65 million residents in Washington, and health department guidance shows that it will likely be April before these groups are able to get vaccinated.
The Department of Health has not finalized Phases 2, 3 or 4 yet, but it will be well into summer before there is enough vaccine for all Washington residents who want it, current estimates show.
Howard suggested patience in the meantime, as well as selflessness, to ensure that those who are most vulnerable to getting the virus and suffering most from it are protected first.
“Each of us as individuals has to be committed to integrity in terms of how we present ourselves, and where we fall on the vaccine schedule, and kind to one another in terms of if we think one group or another group should be vaccinated,” Howard said.