Carbon monoxide invisible killer
The human body depends on oxygen to burn fuel (food) and to function. Once oxygen enters the lungs it combines with hemoglobin in the blood. When saturated with oxygen, it is called oxyhemoglobin. After being carried by the bloodstream to the body’s cells, oxyhemoglobin releases oxygen to the tissues.
Carbon monoxide is dangerous because it bonds much more tightly to the hemoglobin than does oxygen. Once hemoglobin combines with carbon monoxide to form carboxyhemoglobin, its ability to combine with oxygen is completely lost. As more carboxyhemoglobin is formed, the amount of oxygen carried to the cells and organs in the body decreases.
Carbon monoxide starves the blood of oxygen, causing the body to suffocate from the inside out. When the carboxyhemoglobin concentration reaches a certain level, people get nauseous, become unconscious, and ultimately die. How quickly symptoms appear depends upon the concentration of carbon monoxide and the duration of exposure. A person’s size, age and health condition also are factors in how quickly effects of carbon monoxide will become evident.
Carbon monoxide (CO) is a colorless, odorless and tasteless poison gas that can be fatal when inhaled. It is sometimes called the “silent killer.” Carbon monoxide is the product of incomplete combustion. As mentioned, carbon monoxide inhibits the blood’s capacity to carry oxygen. CO can be produced when any fossil fuel is burned: gasoline, propane, natural gas, oil or wood.
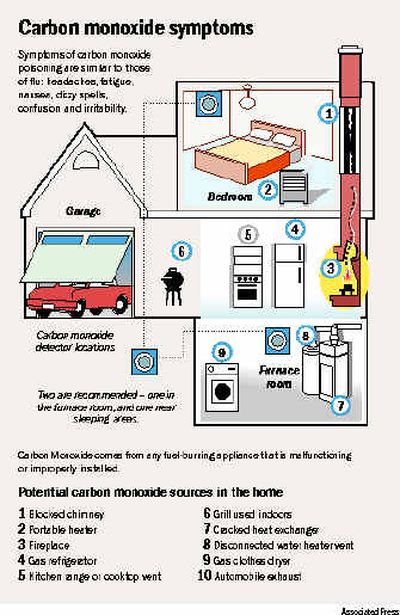
Carbon monoxide comes from fuel-burning appliances that are malfunctioning or improperly installed, including:
• Furnaces
• Gas ranges and stoves
• Gas clothes dryers
• Water heaters
• Portable fuel-burning space heaters
• Fireplaces and wood-burning stoves
Other possible sources include:
• Vehicles and other combustion engines running in an attached garage
• Blocked chimneys or flues
• Cracked or loose furnace exchangers
• Back drafting and changes in air pressure
• A barbecue grill operated in an enclosed space
You need to be diligent about detecting the presence of carbon monoxide in your home. Do so with a carbon monoxide detector.
And, there is another means of detection — human symptoms. This is not how you will want to detect CO. However, it’s important to be familiar with the symptoms of carbon monoxide poisoning.
When exposure is mild, symptoms can include:
• Slight headache
• Nausea
• Vomiting
• Fatigue and/or weakness
• Dizziness
• Disorientation or confusion
When exposure is medium, symptoms can include:
• Throbbing headache
• Drowsiness
• Confusion
• Fast heart rate
When exposure is high, symptoms can include:
• Convulsions
• Unconsciousness
• Brain damage
• Heart and lung failure followed by death
Those most susceptible include:
• Unborn babies
• Young children
• Pregnant women
• Senior citizens
• People with heart or respiratory problems
If you experience even mild CO poisoning symptoms, immediately consult a physician.
Besides installing and maintaining your CO detector, there are other ways to deal with carbon monoxide:
• Every year have the heating system, vents, chimney, and flue inspected by a qualified technician.
• Regularly examine vents and chimneys for improper connections, visible rust and stains.
• Install and operate appliances according to the manufacturer’s instructions.
• Purchase appliances that have been approved by a testing laboratory.
• Never use a gas range or stove to heat the home.
Most detectors that measure carbon monoxide can be placed anywhere in a room.
If the alarm does go off or if anyone displays the above symptoms, get him or her into fresh air immediately and call 911 from a neighbor’s home or on a cell phone.